 A Dowager's hump, also known as kyphosis or hyperkyphosis, refers to an excessive outward curvature of the upper spine, resulting in a rounded hump-like appearance in the upper back and neck. While reversing a Dowager's hump entirely is not always possible, there are measures individuals can take to improve posture, strengthen muscles, and potentially reduce the prominence of the hump. The best medicine of course would be the avoidance of developing such a hump in the first place. A hyperkyphosis can lead to other significant problems such as headaches, neck pain, numbness/tingling, spinal stenosis, disc herniations/bulges, spinal degeneration and arthritis. Prevention and Management Strategies 1. Posture Correction:
0 Comments
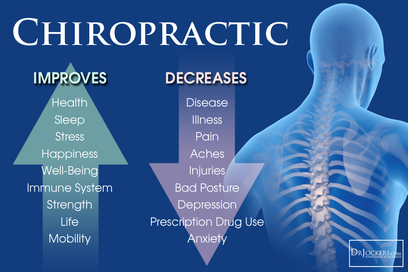
 Image by pressfoto on Freepik Image by pressfoto on Freepik In our quest for optimal health and wellness, we often focus on nutrition, exercise, and mindfulness practices. However, there's one crucial aspect of wellness that is sometimes overlooked: chiropractic maintenance care. Chiropractic care isn't just for alleviating pain; it's a cornerstone of preventive healthcare that can unlock a host of benefits for both body and mind. Chiropractic care is founded on the principle that proper alignment of the spine is essential for the body to function optimally. Through adjustments and other manual techniques, chiropractors aim to restore alignment, relieve pressure on nerves, and facilitate the body's natural ability to heal itself. While many people seek chiropractic care to address specific issues like back pain, neck pain, or headaches, maintenance care takes a proactive approach. Rather than waiting for symptoms to arise, individuals engage in regular chiropractic visits to maintain spinal health and prevent future problems. Just as we service our cars regularly to prevent breakdowns, our bodies also benefit from routine maintenance. Here's why regular chiropractic care is so vital:
If you're new to chiropractic care or considering incorporating maintenance visits into your wellness routine, here are a few tips to get started:
TEXT or call 203-842-8631 to schedule your chiropractic "tune-up" today! 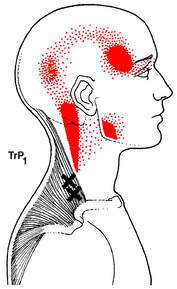 Trigger points (MTrP) are discrete, focal, hyperirritable spots located in a taut band of skeletal muscle. They produce pain locally and in a referred pattern which often accompany chronic musculoskeletal disorders. Acute trauma or repetitive movements may lead to the development of stress on muscle fibers and the formation of trigger points. Patients may have regional, persistent pain resulting in a decreased range of motion in the affected muscles. These include muscles used to maintain body posture, such as those in the neck, shoulders, and pelvic girdle. Trigger points may also manifest as tension headache, tinnitus, temporomandibular joint pain, decreased range of motion in the legs, and low back pain. 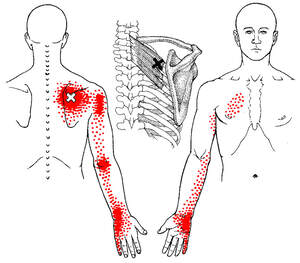 Unfortunately, much of the terminology, theories, concepts, and diagnostic criteria are inconsistent, incomplete, or controversial. U.S. physician Janet Travell, and her partner Rinzler, coined the term “myofascial trigger point” in the 1950s, reflecting their finding that the nodules can be present and refer pain (pain experienced away from the location of the trigger point) to both muscle and overlying fascia. Although the MTrP is a common physical finding, it is often an overlooked component of non-articular musculoskeletal pain because its pathophysiology is not fully understood. In spite of its high prevalence in patients, it is not a commonly established diagnosis, and is considered to be the great imitator.  Research suggests strong evidence supporting chiropractic manipulation, ischemic pressure, and electric stimulation for immediate pain relief at MTrPs. A successful treatment protocol relies on identifying trigger points and elongating the structures affected along their natural range of motion and length by stretching the muscle in conjunction with passive, active, active isolated (AIS), muscle energy techniques (MET), and proprioceptive neuromuscular facilitation (PNF) stretching to be effective. If you, or a loved one, suffers from pain, call our office today at (203) 842-8631 For further questions, e-mail SheltonSportsandSpine@gmail.com Information provided by PubMed®
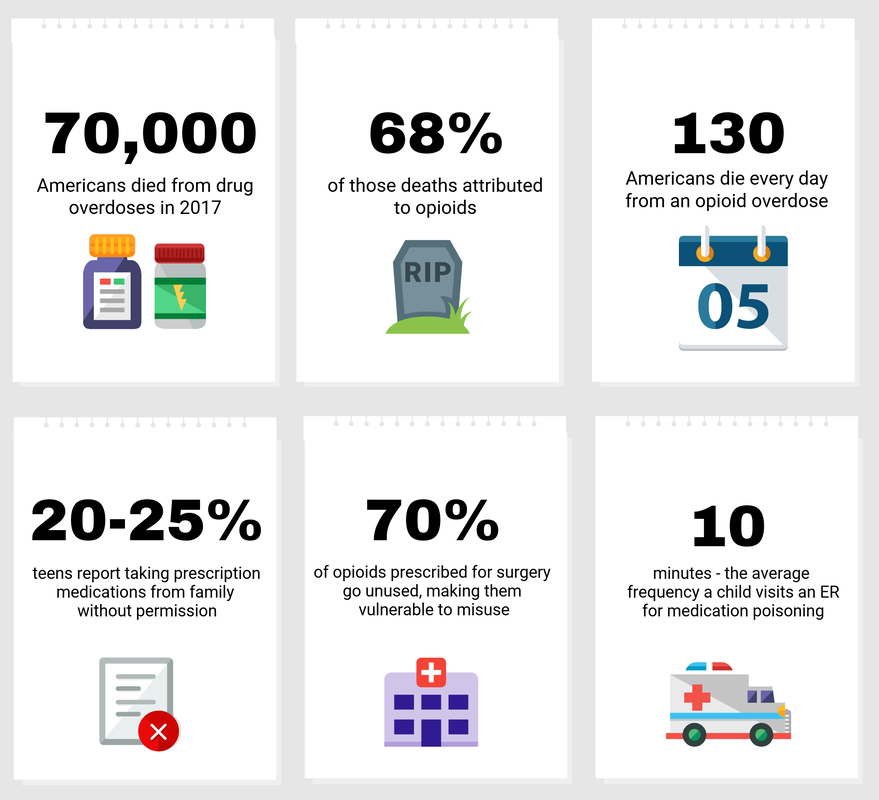
A service of the National Library of Medicine, PubMed® contains publication information and (in most cases) brief summaries of articles from scientific and medical journals. For guidance from NCCIH on using PubMed, see How To Find Information About Complementary Health Approaches on PubMed. Website: www.ncbi.nlm.nih.gov/pubmed Shah JP, Thaker N, Heimur J, Aredo JV, Sikdar S, Gerber L. Myofascial Trigger Points Then and Now: A Historical and Scientific Perspective. PM R. 2015;7(7):746–761. doi:10.1016/j.pmrj.2015.01.024 J Manipulative Physiol Ther. 2009 Jan;32(1):14-24. doi: 10.1016/j.jmpt.2008.06.012. Chiropractic management of myofascial trigger points and myofascial pain syndrome: a systematic review of the literature. Vernon H1, Schneider M.  The synthetic opioid fentanyl, now ubiquitous in the illegal drug market — is increasing. The State Medical Examiner reported in 2019 that there were 1,200 accidental drug deaths; this equates to an 18% spike from the previous year. The opioid crisis has become the worst drug epidemic in modern American history with over 70,000 deaths across the nation. Opioids are drugs that need to be cultivated from a plant, specifically the poppy plant. Once harvested, the dried ruminates of the plant can be manufactured to make morphine, opium, and heroin. This type of opioid has been used for thousands of years, dating back to 3400 BC for medicinal purposes. 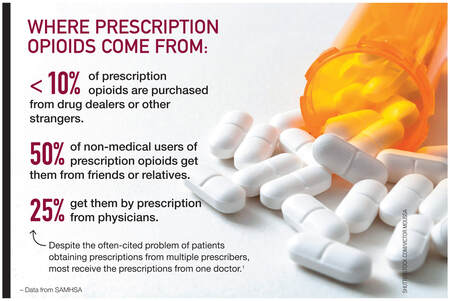 Utilization of nonpharmacological pain management may prevent unnecessary use of opioids. In a retrospective study analyzing back pain patients from 2012-2017 residing in 3 different US states, the study compared the use of primary care intervention versus chiropractic care. The results showed that patients with spinal pain who saw a chiropractor had half the risk of filling an opioid prescription. Among those who saw a chiropractor within 30 days of diagnosis, the reduction in risk was greater as compared with those with their first visit after the acute phase.
If you, or a loved one, suffers from pain, call our office today at (203) 842-8631 For further questions, e-mail SheltonSportsandSpine@gmail.com Information provided by PubMed®
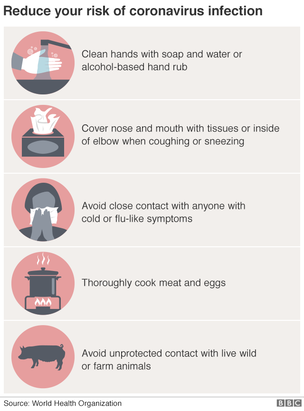
A service of the National Library of Medicine, PubMed® contains publication information and (in most cases) brief summaries of articles from scientific and medical journals. For guidance from NCCIH on using PubMed, see How To Find Information About Complementary Health Approaches on PubMed. Website: www.ncbi.nlm.nih.gov/pubmed Pain Med. 2020 Mar 6. pii: pnaa014. doi: 10.1093/pm/pnaa014. [Epub ahead of print] Impact of Chiropractic Care on Use of Prescription Opioids in Patients with Spinal Pain. Whedon JM1, Toler AWJ1, Kazal LA2, Bezdjian S1, Goehl JM2, Greenstein J3.  Worrying about all the news on the new coronavirus and the illness it causes? Well, that makes good sense. If you often struggle with anxiety, worries about your health, or obsessive thoughts and actions, you might need additional assistance, so we are here to help. Keep these thoughts in mind. You’re fully prepared to help yourself. You can take steps to calm and steady yourself. Remember what works for you — because as fellow humans we’re not so dissimilar, but we do tend to have our own preferences and best practices.
While no one source of information is perfect, some are undeniably better than others! Here are some examples:
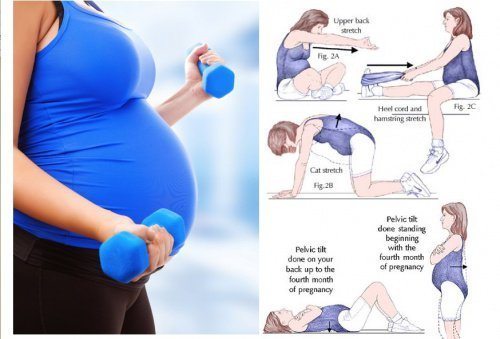
 We’re all on this journey together. News about the virus will likely grow worse, then grow better. Listen to public health experts who can help us navigate the path ahead. Take sensible steps that can help us all: get your bearings, practice good hygiene, use calming strategies that work for you — and maybe try something new. Making healthy, reasonable choices about what to do and what not to do will make a big difference in being able to stay as safe and as well as possible.  75 percent of pregnant women experience pregnancy-related low back pain, pelvic pain, or a combination; this pain increases as pregnancy progresses. In an effort to avoid chemically treating your symptoms, why not manage them with an effective drugless alternative? With the unavoidable change in your center of gravity, this process increases your lumbar lordosis, resulting in musculoskeletal conditions. 2. Sciatic Nerve Pain: since your precious cargo contributes to uterine pressure on supporting vasculature or direct compression of the sciatic nerve. 3. Sacral Pain: as hormonal changes allow for ligament laxity, increased mobility, and joint separation from Relaxin. Pubis dysfunction can produce pain and unwanted symptoms during the birthing process. Chiropractic care and patient education as part of a comprehensive prenatal care team has been shown to hold greater benefit for pregnant patients than traditional obstetric care alone. If you are experiencing debilitating low back pain as a result of pregnancy, call or text (203) 842-8631 to receive the best evidence based treatments that effectively treat and prevent these pesky symptoms. Information provided by PubMed®
A service of the National Library of Medicine, PubMed® contains publication information and (in most cases) brief summaries of articles from scientific and medical journals. For guidance from NCCIH on using PubMed, see How To Find Information About Complementary Health Approaches on PubMed. Website: www.ncbi.nlm.nih.gov/pubmed Weis CA, et al. Prevalence of Low Back Pain, Pelvic Girdle Pain, and Combination Pain in a Pregnant Ontario Population. J Obstet Gynaecol Can. 2018 Aug; 40(8): 1038-1043. https://www.ncbi.nlm.nih.gov/pubmed/30103876 Lisi AJ. Chiropractic spinal manipulation for low back pain of pregnancy: a retrospective case series. J Midwifery Womens Health 2006; 51:7-10. https://www.ncbi.nlm.nih.gov/pubmed/16399602 George JW, Skaggs CD, Thompson PA, et al. A randomized controlled trial comparing a multimodal intervention and standard obstetrics care for low back and pelvic pain in pregnancy. Am J Obstet Gynecol 2013;208:295.e1-7. https://www.ajog.org/article/S0002-9378(12)01969-2/fulltext
 Many of us expect guidance from the local orthopedist; with advice from a trusted source, it is advised to pursue a course of physical therapy. Acute pain is a complex process involving activation of: nociceptors, chemical mediators, and inflammation. Both prescribed and over-the-counter medications can target elements within the pain pathway to eliminate or reduce the sensation of symptoms. Pain management begins, when possible, prior to the tissue trauma until acute pain is appropriately managed. Clinical outcomes and satisfaction most likely will be improved.
 Even medication or physical modalities are "palliative care", and symptoms can be expected to persist if the underlying cause goes untreated. Research shows that cervical traction in conjunction of transcutaneous electrical stimulation demonstrates both analgesic efficacy with improved global mobility/pain levels with cervical disorders. [1] If you or someone you know suffers from debilitating neck pain, call or text (203) 842-8631 to receive the best evidence based treatments that effectively treat and prevent these pesky symptoms. Information provided by PubMed® A service of the National Library of Medicine, PubMed® contains publication information and (in most cases) brief summaries of articles from scientific and medical journals. For guidance from NCCIH on using PubMed, see How To Find Information About Complementary Health Approaches on PubMed. Website: www.ncbi.nlm.nih.gov/pubmed 1. Med Sci Monit. 2017; 23: 335–342.
The Effectiveness of Cervical Spondylosis Therapy with Saunders Traction Device and High-Intensity Laser Therapy: A Randomized Controlled Trial 2. Journal ListMo Medv.110(1); Jan-Feb 2013PMC6179627 A Review of Management of Acute Pain Quinn Johnson, MD
To be continued.... (check out or instagram @DrQChiro for more)What athlete wouldn't want to be able to jump a little higher to get that competitive edge? Would you ever consider going to your Chiropractor if it meant you might be able to increase your vertical jump with an adjustment? It's true! The effect of a chiropractic high-velocity, low-amplitude manipulation in those who suffer from ankle joint dysfunction over a 3 week period had statistically significant improvement in vertical jump height.
 There were no adverse effects in this study, as chiropractic manipulation is non-invasive nor uses pharmacologic intervention to achieve these results. Your feet have an important stability function. If the foundation that you stand on is dysfunctional, these stresses will be transmitted to other parts of your body with discomfort and pain being felt in your ankles, knees and lower back. If you'd like to have our doctors assess you, or someone you know, call or text our office TODAY at (203) 842-8631. Information provided by PubMed®
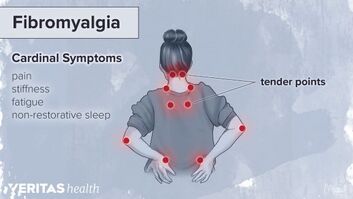
A service of the National Library of Medicine, PubMed® contains publication information and (in most cases) brief summaries of articles from scientific and medical journals. For guidance from NCCIH on using PubMed, see How To Find Information About Complementary Health Approaches on PubMed. Website: www.ncbi.nlm.nih.gov/pubmed J Manipulative Physiol Ther. 2014 Feb;37(2):116-23. doi: 10.1016/j.jmpt.2013.11.004. Epub 2014 Jan 2. Effect of chiropractic manipulation on vertical jump height in young female athletes with talocrural joint dysfunction: a single-blind randomized clinical pilot trial. Hedlund S1, Nilsson H1, Lenz M1, Sundberg T2. Fibromyalgia is the second most common condition affecting your bones and muscles. Yet it's often misdiagnosed and misunderstood. Its classic symptoms are widespread muscle and joint pain and fatigue. There's no cure. But a combination of medication, exercise, managing your stress, and healthy habits may ease your symptoms enough that you can live a normal, active life.  Fibromyalgia can feel similar to osteoarthritis, bursitis, and tendinitis. But rather than hurting in a specific area, the pain and stiffness could be throughout your body. Studies to evaluate resistance training with Chiropractic treatment have proven that this combination of treatment improved strength and reduced symptoms of FM. It also improved adherence to the treatment plan and reduced dropout rates while facilitating greater improvements of the domains of functionality. Information provided by PubMed®
A service of the National Library of Medicine, PubMed® contains publication information and (in most cases) brief summaries of articles from scientific and medical journals. For guidance from NCCIH on using PubMed, see How To Find Information About Complementary Health Approaches on PubMed. Website: www.ncbi.nlm.nih.gov/pubmed J Altern Complement Med. 2009 Mar;15(3):321-8. doi: 10.1089/acm.2008.0132. Effects of resistance training and chiropractic treatment in women with fibromyalgia. Panton LB1, Figueroa A, Kingsley JD, Hornbuckle L, Wilson J, St John N, Abood D, Mathis R, VanTassel J, McMillan V.  The question is often asked whether or not you need to continue to see your Chiropractor after your symptoms have resolved. Aside from spinal manipulation (SMT), Shelton Sports & Spine also offers massage, acupuncture, nutrition, and functional assessments. Spinal manipulation is a common treatment for low back pain, and studies show how effective it can be even when you're not symptomatic. Based on studies, patients who followed-up with their Chiropractor for evaluations and treatment showed more improvement in pain and disability scores. SMT is effective for the treatment of chronic nonspecific LBP. This technique requires the use of the practitioners hands or device to apply a controlled thrust (that is, a force of a specific magnitude or degree in a specific direction) to a joint of your spine. The amount of force can vary, but the thrust allows the joint more mobility than it would on its own. Spinal manipulation is different from spinal mobilization, which doesn’t involve a thrust (and is performed within a joint’s natural range of motion and can be controlled by the patient).
 Spinal manipulation is safe when performed by a trained and licensed practitioner. The most common side effects of spinal manipulation are temporary muscle soreness, stiffness, or a temporary increase in pain. In a 2017 clinical practice guideline, the ACP suggested that spinal manipulation remains a recommended treatment option for chronic low-back pain, due to evidence of effectiveness. Don't wait until your symptoms become bothersome. Call our office today at (203) 842-8631, and together let's continue to achieve your best at our multidisciplinary clinic. Information provided by PubMed®
A service of the National Library of Medicine, PubMed® contains publication information and (in most cases) brief summaries of articles from scientific and medical journals. For guidance from NCCIH on using PubMed, see How To Find Information About Complementary Health Approaches on PubMed. Website: www.ncbi.nlm.nih.gov/pubmed Spine (Phila Pa 1976). 2011 Aug 15;36(18):1427-37. doi: 10.1097/BRS.0b013e3181f5dfe0. Does maintained spinal manipulation therapy for chronic nonspecific low back pain result in better long-term outcome? Senna MK1, Machaly SA.  Even Tufts School of Dental Medicine has acknowledged the significance of the use of Chiropractic care, and have TWO Chiropractors who lecture to current dental students on craniofascial pain. If you and/or someone you know experiences TMJ, call or text our office today to talk to our doctors and therapists on ways we can help at (203) 842-8631.
*J Manipulative Physiol Ther. 2012 Jan;35(1):26-37. doi:10.1016/j.jmpt.2011.09.004. Epub 2011 Nov 10. Intraoral myofascial therapy for chronic myogenous temporomandibular disorder: a randomized controlled trial. Kalamir A1, Bonello R, Graham P, Vitiello AL, Pollard H.
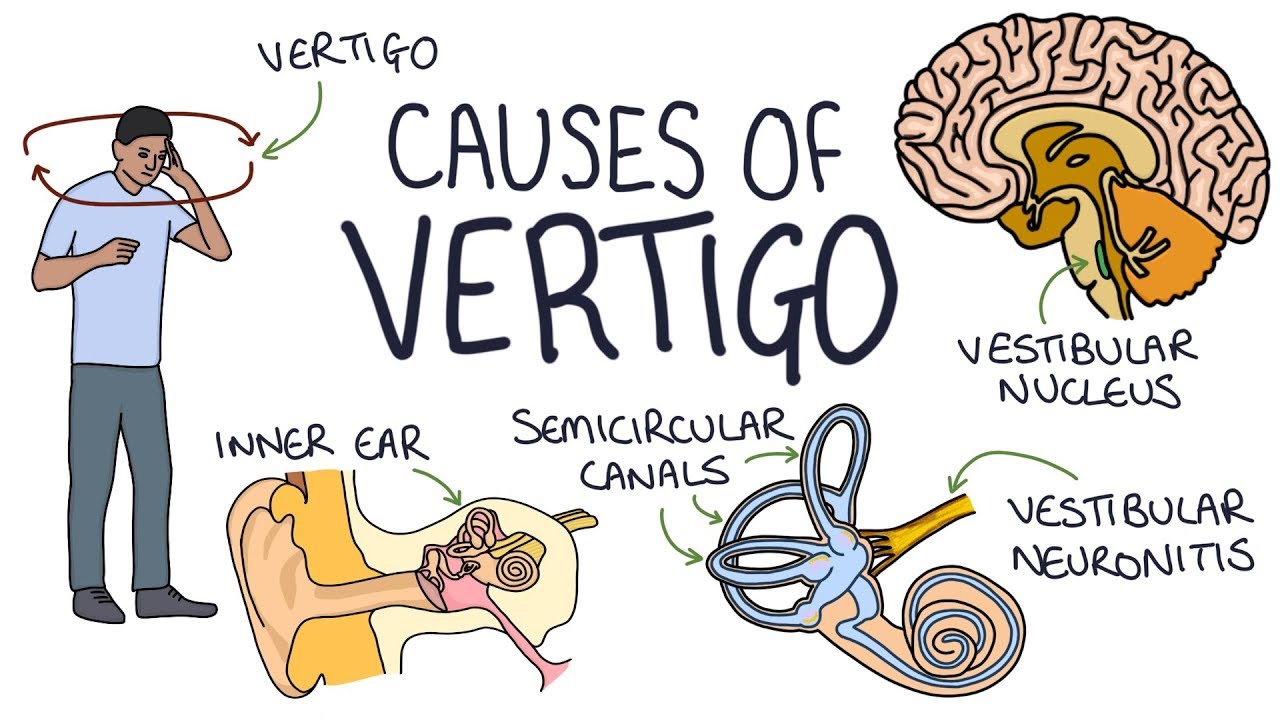
Call or text (203) 842-8631 today if you, or someone you know, is experiencing vertigo. *J Manipulative Physiol Ther. 2013 Feb;36(2):119-26. doi: 10.1016/j.jmpt.2012.12.011.
|
| Who doesn't enjoy restful sleep? The time we spend asleep allows our body to regenerate and repair itself. Due to hectic work schedules and requirement at home, we already don’t get the necessary amount of sleep we need; therefore, it’s in our best interest to minimize possible sleep disturbances whenever we can! It has been shown that 50-60% of adults have reported nocturnal leg cramps. It is most prevalent in the elderly and pregnant population. There is no exact cause for nocturnal leg cramps, but some possibilities include: prolonged sitting, improper posture, and over-exerting muscles in the lower body. | Water is required for biological and physiological processes in our body; and, if we don’t give our body the water it needs, we won’t be able to carry out processes and functions at optimal levels. The National Academies of Sciences, Engineering, and Medicine states an adequate fluid intake level for men is about 15.5 cups a day and 11.5 cups for women |
Exercises to Avoid Nocturnal Cramping and Improve Function:
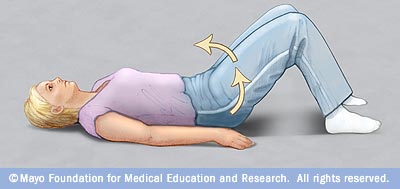
Pelvic Tilt – Find your hip bone and tilt it forward and back. Don’t lift/bridge your hips up, only tilt!

Open Book – Don’t just reach your hand to the bed. Focus on trying to get your shoulder blade as close to the bed as possible.
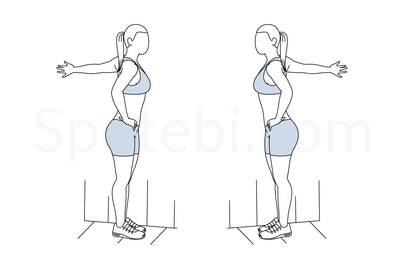
Pec Stretch – Place your elbow at a 45 degree angle with your foot on the same side taking a step in front. Gently push your chest forward to feel a stretch. Hold for 30 seconds.

QL Stretch – With your limbs in position, lean away from the doorway to feel the stretch in your low back.
Sleeping on your stomach can cause issues in the low back, since your spine is put in an unnatural position. If you can’t avoid stomach sleeping, place a small pillow under your pelvis to correct alignment.
Consistent side-sleeping can put your hips out of alignment. You can place a pillow in between your knees to lessen pressure on the hips, but think about transitioning to a better sleep position.
The best way to sleep is on your back! This position keeps your spine neutral and allows to distribute your body weight evenly. If you feel any pressure in the low back due to natural curvature, you can always place a pillow under your knees
If you’re a side sleeper, be cognizant of your neck position. The height of your pillow should allow your neck to be in neutral alignment. The neck is not directly connected to the legs, so how could that affect anything? Cervical spine alignment impacts alignment for the rest of the spine, and the lower spine has more of a direct impact on the leg muscles. Although not in direct proximity to the lower extremity, it has an affect on the entire kinectic chain of our body.
Keep these tips and tricks in mind for nocturnal leg cramp prevention! Call (203) 842-8631 to Schedule an appointment today if you'd like to review these stretches or explore nutritional supplementation to help avoid these symptoms.
Consistent side-sleeping can put your hips out of alignment. You can place a pillow in between your knees to lessen pressure on the hips, but think about transitioning to a better sleep position.
The best way to sleep is on your back! This position keeps your spine neutral and allows to distribute your body weight evenly. If you feel any pressure in the low back due to natural curvature, you can always place a pillow under your knees
If you’re a side sleeper, be cognizant of your neck position. The height of your pillow should allow your neck to be in neutral alignment. The neck is not directly connected to the legs, so how could that affect anything? Cervical spine alignment impacts alignment for the rest of the spine, and the lower spine has more of a direct impact on the leg muscles. Although not in direct proximity to the lower extremity, it has an affect on the entire kinectic chain of our body.
Keep these tips and tricks in mind for nocturnal leg cramp prevention! Call (203) 842-8631 to Schedule an appointment today if you'd like to review these stretches or explore nutritional supplementation to help avoid these symptoms.
We see many patients in our Shelton office who are suffering from acute or chronic pain, and we've found that our chiropractic approach is very successful and getting people relief.
Your body contains roughly 60 different chemicals and each one is responsible for very different functions and regulatory actions. For instance, calcium helps your muscles contract and potassium regulates your heartbeat. Sodium controls the balance of water in your system and fluorine protects your teeth against decay. There are also four chemicals associated with management of pain, and a study published in Journal of Orthopaedic & Sports Physical Therapy has found that chiropractic promotes almost all of them.
Your body contains roughly 60 different chemicals and each one is responsible for very different functions and regulatory actions. For instance, calcium helps your muscles contract and potassium regulates your heartbeat. Sodium controls the balance of water in your system and fluorine protects your teeth against decay. There are also four chemicals associated with management of pain, and a study published in Journal of Orthopaedic & Sports Physical Therapy has found that chiropractic promotes almost all of them.
For purposes of this study, researchers chose thirty participants who weren’t actively in any sort of pain to see what effect chiropractic treatments had on their levels of neurotensin, oxytocin, orexin A, and cortisol—the four chemicals that impact how much pain a person feels. The subjects were separated into three different groups: ten engaged in cervical spinal manipulation (chiropractic involving the neck area), ten received thoracic spinal manipulation (manipulation to the discs and vertebrae in the middle and upper back), and the final ten subjects were the control group, so they received no spinal manipulation therapy whatsoever. Researchers drew each individual’s blood prior to, immediately after, and two hours post-treatment to determine the starting levels of neurotensin, oxytocin, orexin A, and cortisol, as well as to note any changes that may occur.
Immediately upon conclusion of the spinal manipulation sessions, researchers found “significantly higher” levels of both neurotensin and oxytocin in the participants who received either form of spinal manipulation. Cortisol levels increased only for the subjects who engaged in cervical spinal manipulation, and orexin A levels were unaffected by the chiropractic treatments entirely.
Immediately upon conclusion of the spinal manipulation sessions, researchers found “significantly higher” levels of both neurotensin and oxytocin in the participants who received either form of spinal manipulation. Cortisol levels increased only for the subjects who engaged in cervical spinal manipulation, and orexin A levels were unaffected by the chiropractic treatments entirely.
These findings suggest that engaging in regular chiropractic care can help your pain on a cellular level by changing the chemical makeup of your body. Not to mention, regular spinal manipulations also work to correct the spinal issue that is causing the pain in the first place. This makes chiropractic an effective two-prong approach to pain management.
If you're in pain, chiropractic care can help. We've helped hundreds of patients with auto injury pain, sciatica, back pain, neck pain, and more. Don't put your health second, call to schedule your appointment today!
That's a wrap for our blog this week! Stay tuned for our next blog, and send your questions to SheltonSportsandSpine@gmail.com
*Plaza-Manzano G, Molina F, Lomas-Vega R, et al. Changes in biochemical markers of pain perception and stress response after spinal manipulation. Journal Orthopaedic and Sports Physical Therapy 2014;44(4):231-9.
If you're in pain, chiropractic care can help. We've helped hundreds of patients with auto injury pain, sciatica, back pain, neck pain, and more. Don't put your health second, call to schedule your appointment today!
That's a wrap for our blog this week! Stay tuned for our next blog, and send your questions to SheltonSportsandSpine@gmail.com
*Plaza-Manzano G, Molina F, Lomas-Vega R, et al. Changes in biochemical markers of pain perception and stress response after spinal manipulation. Journal Orthopaedic and Sports Physical Therapy 2014;44(4):231-9.
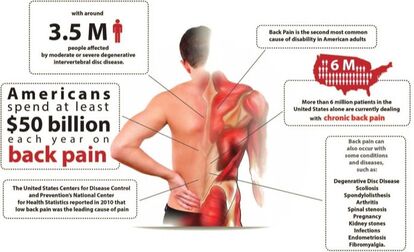
Treatment Recommendations for Low Back Pain Include Chiropractic
| The American College of Physicians (ACP) recommends in an evidence-based clinical practice guideline published today in Annals of Internal Medicine that physicians and patients should treat acute or subacute low back pain with non-drug therapies such as superficial spinal manipulation. If drug therapy is desired, physicians and patients should select nonsteroidal anti-inflammatory drugs (NSAIDs) or skeletal muscle relaxants. |
| Low back pain is one of the most common reasons for all physician visits in the U.S. Most Americans have experienced low back pain. Approximately one quarter of U.S. adults reported having low back pain lasting at least one day in the past three months. Pain is categorized as acute (lasting less than four weeks), subacute (lasting four to 12 weeks, and chronic (lasting more than 12 weeks). “Physicians should reassure their patients that acute and subacute low back pain usually improves over time regardless of treatment,” said Nitin S. Damle, MD, MS, MACP, president, ACP. “Physicians should avoid prescribing unnecessary tests and costly and potentially harmful drugs, especially narcotics, for these patients.” |
For patients with chronic low back pain who have had an inadequate response to non-drug therapy, ACP recommends that physicians and patients consider treatment with NSAIDs as first line therapy; or tramadol or duloxetine as second line therapy. Physicians should only consider opioids as an option in patients who have failed the aforementioned treatments and only if the potential benefits outweigh the risks for individual patients and after a discussion of known risks and realistic benefits with patients.
“Physicians should consider opioids as a last option for treatment and only in patients who have failed other therapies, as they are associated with substantial harms, including the risk of addiction or accidental overdose,” said Dr. Damle.
“Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain” is based on a systematic review of randomized controlled trials and systematic reviews published on noninvasive pharmacological and non-pharmacological treatments of nonradicular low back pain. Clinical outcomes evaluated included reduction or elimination of low back pain, improvement in back-specific and overall function, improvement in health-related quality of life, reduction in work disability/return to work, global improvement, number of back pain episodes or time between episodes, patient satisfaction, and adverse effects.
The evidence was insufficient or lacking to determine treatments for radicular low back pain. The evidence also was insufficient for most physical modalities and for which patients are likely to benefit from which specific therapy. The guideline does not address topical therapies or epidural injection therapies.
ACP’s clinical practice guidelines are developed through a rigorous process based on an extensive review of the highest quality evidence available, including randomized control trials and data from observational studies. ACP also identifies gaps in evidence and direction for future research through its guidelines development process.
ACP’s previous recommendations for treating low back pain were published in “Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society” in 2007. Some evidence has changed since the 2007 guideline and supporting evidence reviews. The 2007 guideline did not assess mindfulness-based stress reduction, MCE, taping, or tai chi
That's a wrap for our blog this week! Stay tuned for our next blog, and send your questions to SheltonSportsandSpine@gmail.com
“Physicians should consider opioids as a last option for treatment and only in patients who have failed other therapies, as they are associated with substantial harms, including the risk of addiction or accidental overdose,” said Dr. Damle.
“Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain” is based on a systematic review of randomized controlled trials and systematic reviews published on noninvasive pharmacological and non-pharmacological treatments of nonradicular low back pain. Clinical outcomes evaluated included reduction or elimination of low back pain, improvement in back-specific and overall function, improvement in health-related quality of life, reduction in work disability/return to work, global improvement, number of back pain episodes or time between episodes, patient satisfaction, and adverse effects.
The evidence was insufficient or lacking to determine treatments for radicular low back pain. The evidence also was insufficient for most physical modalities and for which patients are likely to benefit from which specific therapy. The guideline does not address topical therapies or epidural injection therapies.
ACP’s clinical practice guidelines are developed through a rigorous process based on an extensive review of the highest quality evidence available, including randomized control trials and data from observational studies. ACP also identifies gaps in evidence and direction for future research through its guidelines development process.
ACP’s previous recommendations for treating low back pain were published in “Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society” in 2007. Some evidence has changed since the 2007 guideline and supporting evidence reviews. The 2007 guideline did not assess mindfulness-based stress reduction, MCE, taping, or tai chi
That's a wrap for our blog this week! Stay tuned for our next blog, and send your questions to SheltonSportsandSpine@gmail.com

YES
Understanding Carpal Tunnel:
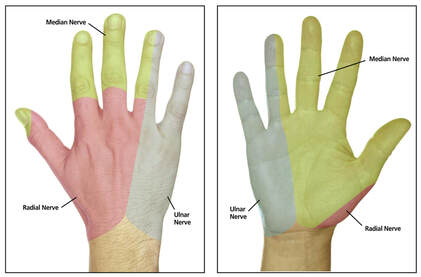
Carpal tunnel syndrome is characterized by numbness, tingling, or pain in the hands (particularly the thumb, index finger, middle finger and the thumb side of the ring finger, as this is the part of the hand innervated by the median nerve). The irritation or pain can also refer up the arm, affecting more than just the hand and wrist. The onset might be during sleep, after prolonged activity, or seemingly random. Persistence or recurrence of these symptoms should definitely be addressed! Un-addressed carpal tunnel will lead to a steady increase in these symptoms, and eventually weakness and atrophy of the hands.
True Carpal Tunnel is an irritation of the median nerve at the transverse carpal ligament. Carpal tunnel affects about 1 in 10 people, making it the most common nerve compression syndrome!
Carpal tunnel syndrome often affects, machinists, hairdressers, musicians, massage therapists, even chiropractors! Anyone making prolonged repetitive use of their hands, fingers and wrists. Now that everyone is texting and typing as much as typists used to when this syndrome was identified... It can really affect anyone.
Understanding Carpal Tunnel:
Carpal tunnel syndrome is characterized by numbness, tingling, or pain in the hands (particularly the thumb, index finger, middle finger and the thumb side of the ring finger, as this is the part of the hand innervated by the median nerve). The irritation or pain can also refer up the arm, affecting more than just the hand and wrist. The onset might be during sleep, after prolonged activity, or seemingly random. Persistence or recurrence of these symptoms should definitely be addressed! Un-addressed carpal tunnel will lead to a steady increase in these symptoms, and eventually weakness and atrophy of the hands.
True Carpal Tunnel is an irritation of the median nerve at the transverse carpal ligament. Carpal tunnel affects about 1 in 10 people, making it the most common nerve compression syndrome!
Carpal tunnel syndrome often affects, machinists, hairdressers, musicians, massage therapists, even chiropractors! Anyone making prolonged repetitive use of their hands, fingers and wrists. Now that everyone is texting and typing as much as typists used to when this syndrome was identified... It can really affect anyone.
Understanding Nerve Compression Syndromes:
When you have symptoms of numbness or tingling, this usually indicates a nerve problem. Nerves run from the spine throughout the body to give us sensation and feeling, giving our brains vital information about the world around us.
When a nerve is compressed or pinched, it interferes with these signals. This is what happens when your arm or foot falls asleep after sitting on it for a long time. Except with carpal tunnel you can’t quite shake it out the way you can a sleeping foot. The more frequent and persistent numbness and tingling become the more severe the problem is.
Carpal Tunnel Syndrome specifically compresses the median nerve at the wrist. There are other syndromes that have the same symptoms as carpal tunnel, for example, the median nerve can be compressed at the elbow such as in pronator teres syndrome, or at the shoulder such as in thoracic outlet syndrome, or in the neck due to a subluxation or misalignment in the cervical spine. That is why it is important to get a proper diagnosis for your symptoms. There have been many cases of patients receiving surgery for carpal tunnel but, the surgery did noting for their symptoms as they actually had one of these other conditions.
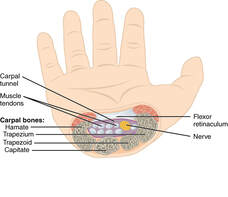
What's happening in the 'tunnel'?
The transverse carpal ligament is a round band of fascia that hold the flexor muscles in place. Imagine a rubbery calamari ring in your wrist, and that your muscles and nerves are strands of spaghetti strands are running through it! (Are you hungry yet?) The wrist is a high traffic area! You’ve got carpal bones, you’ve got the tendons of the flexor muscles, you’ve got the median nerve… When this area gets over-crowded the other tissues in the space will compress the median nerve and cause these symptoms. There are several things that can cause a jam-up in this area include edema, subluxation of a carpal bone, fascial adhesion, inflammation of the flexor muscle tendons, and inflammation of the transverse carpal ligament itself.
Understanding Nerve Compression Syndromes:
When you have symptoms of numbness or tingling, this usually indicates a nerve problem. Nerves run from the spine throughout the body to give us sensation and feeling, giving our brains vital information about the world around us.
When a nerve is compressed or pinched, it interferes with these signals. This is what happens when your arm or foot falls asleep after sitting on it for a long time. Except with carpal tunnel you can’t quite shake it out the way you can a sleeping foot. The more frequent and persistent numbness and tingling become the more severe the problem is.
Carpal Tunnel Syndrome specifically compresses the median nerve at the wrist. There are other syndromes that have the same symptoms as carpal tunnel, for example, the median nerve can be compressed at the elbow such as in pronator teres syndrome, or at the shoulder such as in thoracic outlet syndrome, or in the neck due to a subluxation or misalignment in the cervical spine. That is why it is important to get a proper diagnosis for your symptoms. There have been many cases of patients receiving surgery for carpal tunnel but, the surgery did noting for their symptoms as they actually had one of these other conditions.
What's happening in the 'tunnel'?
The transverse carpal ligament is a round band of fascia that hold the flexor muscles in place. Imagine a rubbery calamari ring in your wrist, and that your muscles and nerves are strands of spaghetti strands are running through it! (Are you hungry yet?) The wrist is a high traffic area! You’ve got carpal bones, you’ve got the tendons of the flexor muscles, you’ve got the median nerve… When this area gets over-crowded the other tissues in the space will compress the median nerve and cause these symptoms. There are several things that can cause a jam-up in this area include edema, subluxation of a carpal bone, fascial adhesion, inflammation of the flexor muscle tendons, and inflammation of the transverse carpal ligament itself.
How can this condition be treated?
Manual therapy can be really effective in treating carpal tunnel. Calming the overworked tissues, reducing inflammation, breaking fascia and adhesions, and reducing pain. Massage, acupuncture, chiropractic adjustment of the wrist, stretches and exercises, using a wrist brace to splint the wrist, resting the wrist, cortisol shots, and even surgery are all options.
If any of the above exercises causes numbness, tingling, or pain in the hands, make an appointment to get checked for carpal tunnel.
Fun Facts:
That's a wrap for our blog this week! We hoped you learned a little more about this common condition. Stay tuned for our next blog, and send your questions to SheltonSportsandSpine@gmail.com
Manual therapy can be really effective in treating carpal tunnel. Calming the overworked tissues, reducing inflammation, breaking fascia and adhesions, and reducing pain. Massage, acupuncture, chiropractic adjustment of the wrist, stretches and exercises, using a wrist brace to splint the wrist, resting the wrist, cortisol shots, and even surgery are all options.
If any of the above exercises causes numbness, tingling, or pain in the hands, make an appointment to get checked for carpal tunnel.
Fun Facts:
- Carpal tunnel syndrome affects more women than men! The exact reason is not exactly understood yet.
- The median nerve, colloquially known as the "eye of the hand"
- Carpal tunnel syndrome is worse for many at night... We are unable to control to position of our wrist while sleeping, many people naturally sleep in a position that folds the hand forward... Compressing the median nerve!
- The first report of median nerve compression recorded was in 1854 by Sir James Paget. Though, Carpal Tunnel Syndrome became more widely diagnosed and discussed in the years following WWII
That's a wrap for our blog this week! We hoped you learned a little more about this common condition. Stay tuned for our next blog, and send your questions to SheltonSportsandSpine@gmail.com

Yes!
Chiropractic has been proven to help manage both acute and chronic pain.
Pain management, in general, is a big issue in healthcare. Let’s look at some facts:
Low back pain is the single leading cause of disability. According to the US bone and Joint initiative study, back pain was cause for over 264 million days off of work. That is all without considering any other type of chronic pain condition. Pain affects more Americans than diabetes, heart disease and cancer combined.
When looking for solutions to chronic pain, the first thing we tend to reach for is over-the-counter aids such as Aspirin, Advil, or Ibuprofen. Then if these conditions worsen and we go to the doctor we are typically directed to stronger prescription medications, which, can be concerning to many patient situations.
Many people are looking for ways to treat their chronic pain without resorting to drugs of the traditional medication protocol. With alternative care we can lessen our dependency on over the counter drugs and even opioids.
Back pain is also one of the most common conditions that opioids are prescribed for with over half of opioid users reporting back pain among their symptoms. Why is this connection between back pain and opioids so concerning?
While prescription opioids are certainly helpful to many patients in complex severe conditions, however, we need to also be looking at the big picture of the opioid crisis: In 2016, illicit and prescription opioids were responsible for more than 42,000 fatal overdoses across the country. According to the Centers of Disease Control and Prevention, those numbers have quintupled since 1999, which means the problem is just getting worse.
The good news is that, alternative medicines are already making great improvements to these dire statistics.
Let's take a look at some strategies the VA has been using in order reduce opioid addiction among veterans. After launching one initiative, they were able to reduce overall opioid prescriptions by 41% over the past five years. The project was focused on non-drug treatment for chronic pain, such as acupuncture, spinal manipulation therapy, chiropractic care, and yoga.
It is also good news to know that patients who received services from a chiropractor were less likely to fill a prescription for opioid medication, and, there was a 51 percent lower likelihood of an adverse drug incident compared to non recipients of chiropractic care.
A visit to the chiropractor may also be more cost effective for sufferers of chronic pain. In one study, "those who initiated treatment for low back pain with chiropractic rather than a regular MD had 40% in reduced healthcare cost!" In general “Healthcare plans that incorporate chiropractic typically realize a 2:1 return for every dollar spent.”
There are numerous research studies, reports, and surveys proving how effective chiropractic can be for pain:
"In a Randomized controlled trial, 183 patients with neck pain were randomly allocated to manual therapy (spinal mobilization), physiotherapy (mainly exercise) or general practitioner care (counseling, education and drugs) in a 52-week study. The clinical outcomes measures showed that manual therapy resulted in faster recovery than physiotherapy and general practitioner care. Moreover, total costs of the manual therapy-treated patients were about one-third of the costs of physiotherapy or general practitioner care."
Korthals-de Bos et al (2003), British Medical Journal
“Patients with chronic low-back pain treated by chiropractors showed greater improvement and satisfaction at one month than patients treated by family physicians. Satisfaction scores were higher for chiropractic patients. A higher proportion of chiropractic patients (56 percent vs. 13 percent) reported that their low-back pain was better or much better, whereas nearly one-third of medical patients reported their low-back pain was worse or much worse.”
Nyiendo et al (2000), Journal of Manipulative and Physiological Therapeutic
The evidence and anecdotes are solid. If you are suffering form chronic or acute pain, chiropractic care may well worth a try!
Send us your questions! Yours might be answered next week. SheltonSportsandSpine@gmail.com
Sources and Further Reading:
NIH Fact Sheet -- Pain Management
The Center for Disease Control and Prevention -- Drug Overdose Deaths
VHA Pain Management -- Opioid Saftey Initiative
Boss Magazine -- Corrective Care for the Opioid Epidemic
American Chiropractic Association -- What Research Shows About Chiropractic
Chiropractic has been proven to help manage both acute and chronic pain.
Pain management, in general, is a big issue in healthcare. Let’s look at some facts:
Low back pain is the single leading cause of disability. According to the US bone and Joint initiative study, back pain was cause for over 264 million days off of work. That is all without considering any other type of chronic pain condition. Pain affects more Americans than diabetes, heart disease and cancer combined.
When looking for solutions to chronic pain, the first thing we tend to reach for is over-the-counter aids such as Aspirin, Advil, or Ibuprofen. Then if these conditions worsen and we go to the doctor we are typically directed to stronger prescription medications, which, can be concerning to many patient situations.
Many people are looking for ways to treat their chronic pain without resorting to drugs of the traditional medication protocol. With alternative care we can lessen our dependency on over the counter drugs and even opioids.
Back pain is also one of the most common conditions that opioids are prescribed for with over half of opioid users reporting back pain among their symptoms. Why is this connection between back pain and opioids so concerning?
While prescription opioids are certainly helpful to many patients in complex severe conditions, however, we need to also be looking at the big picture of the opioid crisis: In 2016, illicit and prescription opioids were responsible for more than 42,000 fatal overdoses across the country. According to the Centers of Disease Control and Prevention, those numbers have quintupled since 1999, which means the problem is just getting worse.
The good news is that, alternative medicines are already making great improvements to these dire statistics.
Let's take a look at some strategies the VA has been using in order reduce opioid addiction among veterans. After launching one initiative, they were able to reduce overall opioid prescriptions by 41% over the past five years. The project was focused on non-drug treatment for chronic pain, such as acupuncture, spinal manipulation therapy, chiropractic care, and yoga.
It is also good news to know that patients who received services from a chiropractor were less likely to fill a prescription for opioid medication, and, there was a 51 percent lower likelihood of an adverse drug incident compared to non recipients of chiropractic care.
A visit to the chiropractor may also be more cost effective for sufferers of chronic pain. In one study, "those who initiated treatment for low back pain with chiropractic rather than a regular MD had 40% in reduced healthcare cost!" In general “Healthcare plans that incorporate chiropractic typically realize a 2:1 return for every dollar spent.”
There are numerous research studies, reports, and surveys proving how effective chiropractic can be for pain:
"In a Randomized controlled trial, 183 patients with neck pain were randomly allocated to manual therapy (spinal mobilization), physiotherapy (mainly exercise) or general practitioner care (counseling, education and drugs) in a 52-week study. The clinical outcomes measures showed that manual therapy resulted in faster recovery than physiotherapy and general practitioner care. Moreover, total costs of the manual therapy-treated patients were about one-third of the costs of physiotherapy or general practitioner care."
Korthals-de Bos et al (2003), British Medical Journal
“Patients with chronic low-back pain treated by chiropractors showed greater improvement and satisfaction at one month than patients treated by family physicians. Satisfaction scores were higher for chiropractic patients. A higher proportion of chiropractic patients (56 percent vs. 13 percent) reported that their low-back pain was better or much better, whereas nearly one-third of medical patients reported their low-back pain was worse or much worse.”
Nyiendo et al (2000), Journal of Manipulative and Physiological Therapeutic
The evidence and anecdotes are solid. If you are suffering form chronic or acute pain, chiropractic care may well worth a try!
Send us your questions! Yours might be answered next week. SheltonSportsandSpine@gmail.com
Sources and Further Reading:
NIH Fact Sheet -- Pain Management
The Center for Disease Control and Prevention -- Drug Overdose Deaths
VHA Pain Management -- Opioid Saftey Initiative
Boss Magazine -- Corrective Care for the Opioid Epidemic
American Chiropractic Association -- What Research Shows About Chiropractic
A: This question is a preemptive strike. When April and May come around, people always ask for tips, tricks, and exercises to help get a nice summer 6 pack to take to the beach.
My answer is usually… Start in February!
The exercises we typically assign to build core muscles such as pelvic tilts, glute bridges, planks, and side-planks are extremely effective. Don’t forget to constantly engage your core doing any exercise, standing, sitting, walking, or running to build your core and help your posture.
Let’s take it up a notch with our PTA, Stuart, who suggests we strengthen our core with hanging exercises. Get off the floor and find somewhere to hang out until summer!
Level 1: Just hang! To do an ‘active hang’ get a good grip on the bar. Engage your shoulders and ‘shrug’ to lift your torso. Straighten your legs and hold them together in a pike. You can engage your legs more pushing your toes into a ‘pointe’ or pulling them up into a ‘flex’ position. Tighten your core and make sure your spine is straight and your hips are aligned with your torso the way you would with a plank. When you can hold this position for 30-60 seconds, move on to the next progression.
In addition to working your core muscles, these hangs also help to decompress the spine, stretch the chest, shoulders, and arms, plus strengthen your hands and grip.
Level 2: Knees to chest. Start in your active hang position, then, keeping your legs and ankles together slowly bend your knees and draw them up towards your chest. Go as high as you can while maintaining your core. Feel free to start with partial-lift, until you work up to getting your knees higher. Want to make it harder? Lift yourself into a pull up or chin up position while bringing your knees up!
Level 3: Straight leg raises. Remember, going slowly and holding your core properly will pay off way more than trying to force the ‘L’ and sacrifice your form. If you can only lift your feet up a few inches at a time, that is still a great start and a great core exercise. Eventually, as you build your strength and flexibility, you will be able to hit that perfect ‘L’ shape. Want to change it up? Try alternating leg lifts, remember to keep both legs pipe-straight, this will work flexibility and strength in each leg individually, and engage your obliques as you work to keep balance.
Because you are hanging and not on the ground you are working all your core muscles together, not just one side at a time. It’s a nice change of pace to traditional sit ups and crunches.
Check out Stuart in the video below for a demonstration of each progression.
I want to stress that the right exercises are only half (that's being generous) of the 6 pack pie, the other aspect is DIET. Good abdominal muscles and core strength are made in the gym, but a great 6 pack is made in the kitchen.
Stay tuned for more exercise articles. Do you have a question about building core strength? Email your question to SheltonSportsandSpine@gmail.com, it might be featured in our next Q & A!
Author
The Shelton Sports & Spine Blog is for answering your questions! Stay tuned to learn about our practice, health, food, treatments, and more!
Archives
April 2024
April 2020
March 2020
February 2020
January 2020
December 2019
November 2019
October 2019
September 2019
August 2019



















 RSS Feed
RSS Feed